Cholangiocarcinoma or bile duct cancer: how to Manage???
Cholangiocarcinoma or bile duct cancer is a cancer of bile
duct. In the past it was considered as untreatable but now due to improvement
in surgical techniques, it can be cured if it is diagnosed and treated in time.
Most
patients are diagnosed after the age of 65, with a peak incidence occurring
during the eighth decade of life. Unlike gallbladder cancer, men appear to have
cholangiocarcinoma slightly more frequently than women. Known risk factors
include
·
primary sclerosing cholangitis
·
choledochal cyst disease
·
chronic biliary parasitic infestation
·
and numerous chemicals, including thorotrast, asbestos, dioxin, and
nitrosamines.
Bile duct cancers are usually of three types:
1.
Intrahepatic or those who arise from bile ducts
insider the liver.
2.
Hilar cholangiocarcinoma or klatskin tumor which
arise generally from the junction of right and left sided bile ducts.
3.
Lower bile duct cancer.
Out of these 3 types hilar cholangiocarcinoma are most
common and most difficult to treat and today we will discuss mostly hilar
cholangiocarcinoma
For hilar cholangiocarcinoma most commonly following
classification system suggested by bismuth is used.
Type 1; Tumor below junction of right and left bile duct
Type 2: Tumor at the junction of right and left bile duct
but not involvement them
Type 3 A: Tumor at the junction of right and left bile duct
plus involving right
Type 3B: Tumor at the junction of right and left plus
involving left
Type 4L tumor involving right and left bile duct as well as
junction
Presentation
or clinical features:
Symptoms
associated with intrahepatic cholangiocarcinomas are nonspecific, including
malaise and abdominal pain. Unlike hilar and distal cholangiocarcinomas, a
minority of patients develop jaundice. Hilar and distal cholangiocarcinomas can
present with nonspecific symptoms of pain, anorexia, and weight loss. Itching is
a common symptom for patients with extrahepatic cholangiocarcinoma, and it
typically precedes clinically apparent jaundice.
It
is jaundice or the presence of abnormal liver enzymes that usually prompts
medical attention.
The
level of jaundice can be informative in distinguishing benign from malignant
biliary obstruction; benign causes of obstructive jaundice typically produce
bilirubin levels ranging from 2 to 4 mg/dL (rarely exceeding 15 mg/dL), whereas
biliary obstruction from cholangiocarcinoma usually results in serum bilirubin
levels greater than 10 mg/dL (with a mean level of approximately 18 mg/dL).
Diagnosis:
Apart
from abovementioned clinical features diagnosis is usually achieved by imaging
modalities suc as CT scan and MRI with
MRCP. Some times endoscopic ultrasound or ERCP are necessary.
Preoperative
MRCP:
Treatment:
Surgical
treatment is the only hope for cure in cases of cholangiocarcinoma.
ALL the cholangiocarcinoma
except mentioned in following table are operable.
Criteria for Unresectability for Cholangiocarcinoma
Medical contraindication to surgical
intervention
Advanced cirrhosis/portal hypertension
Bilateral second-order biliary
Main portal vein involvement
Liver Lobar atrophy with other side
second-order biliary radicle involvement
Liver Lobar atrophy with other side portal
vein involvement
Advanced lymphnode involvement
Distant spread.
Surgery:
The goal of surgical therapy for cholangiocarcinoma
is complete R0 resection. Complete resection has consistently proven to
correlate well with survival.
Hilar Cholangiocarcinoma:
partial liver resection is
often necessary in addition to extrahepatic biliary excision for complete
resection of extrahepatic cholangiocarcinoma. Review of the relevant literature suggests
that the rate of negative-margin resection (no cancer remaining in the body)
closely approximates the frequency with which liver resection is performed. That
means that chances of completely removing the cancer increase when liver
resection done along with cholangiocarcinoma.The proximity of the caudate lobe
of liver to the cancer often mandates concomitant caudate lobe removal; this is
particularly evident for left-sided hilar tumors, as the major caudate lobe bile
ducts drain into the left hepatic bile duct.
Patients
undergoing resection exhibited an overall median survival of 35 months; predictors of improved survival were
· well-differentiated tumors (good cancer biology)
· negative resection margin (no cancer remaining)
· the performance of a concomitant liver resection.
The
importance of obtaining negative resection margins is underscored by the
observation that patients with histologically positive margins (microscopic
cancer inside the body ) of resection demonstrated poor survival outcomes
indistinguishable from those with locally advanced tumors undergoing operative
exploration without attempted resection.
It
appears that the performance of liver resection at the time of resection of
hilar cholangiocarcinoma is critical for optimizing outcome.
Indeed, the 5-year actuarial survival among
those patients undergoing partial liver resection was 37%, compared with 0% for
those treated with bile duct excision alone.
Liver Transplant
Orthotopic liver transplant for cholangiocarcinoma, often done for
patients with underlying primary sclerosing cholangitis, has traditionally been
associated with suboptimal survival outcomes. Recently, the Mayo Clinic has
demonstrated promising results among a select cohort of patients undergoing
neoadjuvant chemoradiation followed by cadaveric or living donor liver
transplant.
Role of
preoperative biliary drainage:
For optimal results and to safely perform major liver resection
particularly in cases of cholangiocarcinoma preoperative biliary drainage
should be done to decrease bilirubin level less than 5.
Because when bilirubin is higher than than it means that liver is
not functioning properly so there are increase chances of infection and post
operative liver failure in this group of patients.
Preoperative biliary drainage:
Management of cholangiocarcinoma according to bismuth
classification:
Intra
Hepatic+ Upper third
Cholangiocarcinomas
without
vascular involvement
Type I, II,
IIIA
Extended right
lobe liver resection with
Caudate lobe
Type III B
Left /Extended
left liver resection
preferably with
caudate resection
For TYPE IV consider liver
transplantation according to mayo protocol
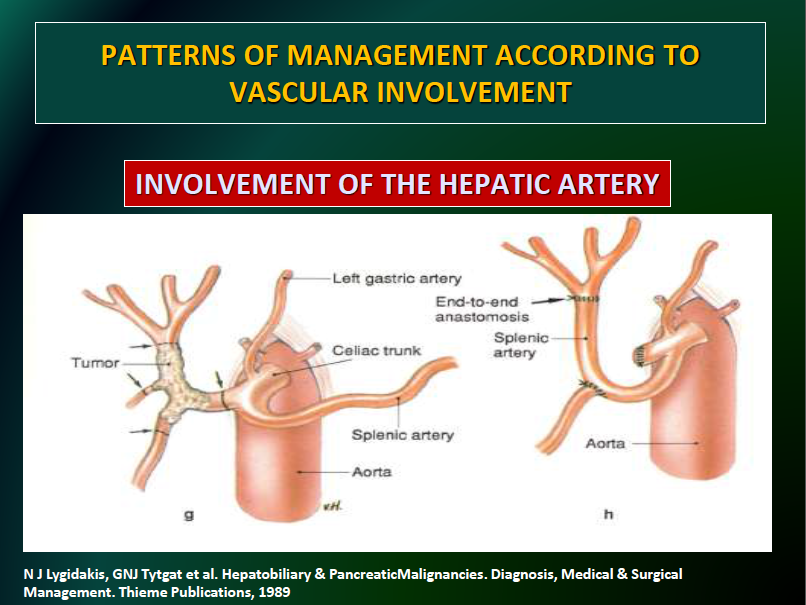
Intra
Hepatic+ Upper Third
Cholangiocarcinomas
with
vascular involvement :
Liver
Resection with Blood vessels resection and reconstruction (if artery/vein
inseparable from tumor and achieves margin –ve
resection)
Initially it
was thought that if tumor involves vessels surgical treatment should not be
offered but now it has been proven that with vessles involvement also surgical
resection can be offered. With these approaches we can achieve 5 year survival
of around 40-50% in these advanced cases also.
Details
mentioned in subsequent figures.
Extended right
hepatectomy
Here I am
posting some pics of extended right liver resection with vascular
reconstruction to give you some idea how extensive surgical approach can save
life.